An overdose occurs when someone takes a toxic amount of one or more substances, which cause the body to be unable to maintain or monitor functions necessary for life. These include breathing, heart rate and regulating body temperature. Not everyone who overdoses will die; however there can be long-term medical impacts from overdose (BCCDC). An overdose depends on a number of factors. For example, with an Opiate overdose, breathing is the primary bodily function affected. As the overdose progresses it may affect heart and other vital bodily functions.
 Three Key Things
Three Key Things
Nalox-what?
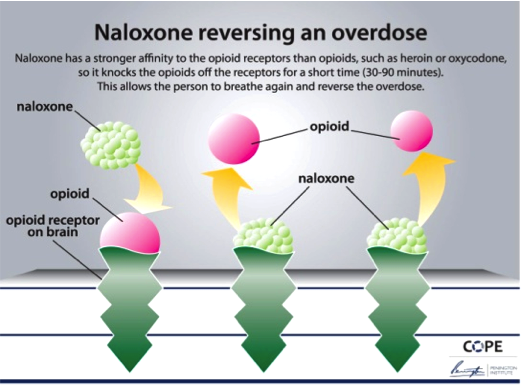
Naloxone, (in Canada) is the injectable form synthetic opioid antagonist used for the reversal of opioid-induced overdoses. Narcan is the name of the nasaly-administrated synthetic opioid antagonist, used for the reversal of opioid-induced overdoses. For the purpose of this course, we will be referring to Naloxone, as Narcan is currently unavailable due to its high cost.
Where Can I Get It?
Your site or facility will be set up as as Take Home Naloxone (THN) distributing site through Toward the Heart, BCCDCs harm-reduction program. Toward the Heart will provide you with THN kits that look like this:
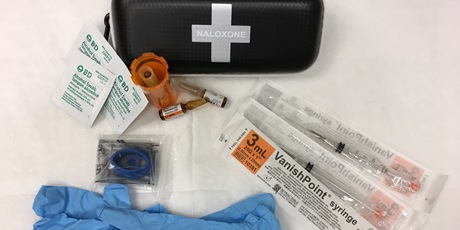
THN kits are then distributed to those at risk of an opiate overdose, or those who may witness an overdose, such as friends and family.
For VCH staff, your manager or employer will decide if your individual role requires carrying a naloxone kit and/or if your team (i.e. outreach) needs a certain number of Naloxone kits per shift. Your manager will then order VCH-funded Naloxone kits (usually blue) to use, while you are on shift. For more details see the Overdose Emergency Response VCH intranet page
How Does It Work?
Naloxone temporarily knocks opioids off their receptors, blocking their action for approximately 20-90 minutes. Depending on the amount and type of opioids taken, a person can be at risk for a repeated overdose after Naloxone has worn off.
 Find Out More
Find Out More
What are the signs and symptoms of an opioid overdose?
- Slow or no breathing
- Gurgling/snoring
- Unable to stay awake
- No response to voice, gentle stimulation, or to pain stimulation (such as a sternal rub)
- Slow or no pulse
- Skin looks pale or grey, blue to lips and/or nails, feels cold
- Small pupils or eyes rolled back
What do I do next? If you witness or find someone who is experiencing an overdose, CALL 911 IMMEDIATELY and follow the SAVE ME steps.
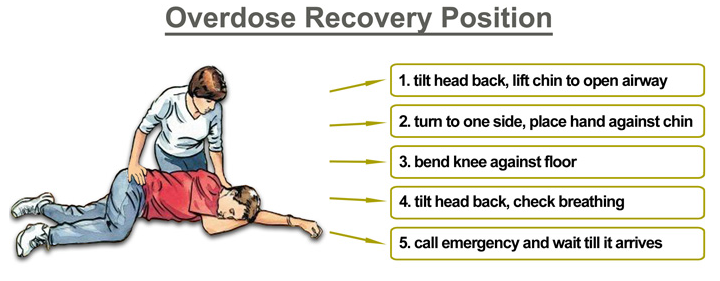
NOTE: In some opioid overdoses, drugs such as methadone have a much longer half-life in the body (meaning that they take longer to be metabolized), than Naloxone, and there is a potential for a secondary overdose. This is why it is important to call 911 immediately. If you need to leave an unconscious/unresponsive person alone at any time, it is important to put them in the recovery position (Click + to see image). The recovery position helps keep the airway clear from obstruction by the tongue or vomit. Be aware that a person experiencing an opioid overdose may in fact experience side effects similar to an opioid withdrawal; nausea, vomiting, diarrhea, muscle aches, etc.
You can learn more about Naloxone administration online, at Toward the Heart.
I’ve been told I can get a free Naloxone kit from BCCDC.
In order to receive a Naloxone kit at no charge, from a BCCDC-approved THN site, you must have completed the THN Training and be at risk of an opioid overdose or must be a friend or family member of a person at high risk of an opioid overdose. Regardless of eligibility for a free kit, you are encouraged to learn how to prevent, recognize and respond to an opioid overdose.
 In Practice
In Practice
David has abstained from using stimulants for the past 3 months. Therefore he doesn’t think he’s at risk for an overdose when he decides to smoke crack cocaine.
What puts David at increased risk of an overdose?
1) a decreased tolerance for drugs due to abstinence or a period of non-use
2) the potential for stimulants to be contaminated by opoids when used by any route
3) David is not at risk for an overdose because he is using stimulants and not opiates
That's right! People who use illicit drugs other than opioids are at risk for contamination. Also people do not have to be currently using; periods of abstinence place someone at high risk for an overdose because anytime someone takes a break from using a substance, their tolerance goes down and it takes a smaller amount of the same substance to get high.
Incorrect - people who use illicit drugs other than opioids are at risk for contamination/ Also people do not have to be currently using; periods of abstinence place someone at high risk for an overdose because anytime someone takes a break from using a substance, their tolerance goes down and it takes a smaller amount of the same substance to get high.
Your client Susan wants to get a take home Naloxone kit for use at her non-profit workplace.
People who want naloxone at their “non-profit” workplace are not eligible for the individual BCCDC THN kits. They must first get employer approval, and then apply through the BC Facility Overdose Response Box (FORB) program at http://towardtheheart.comnaloxone/forb/
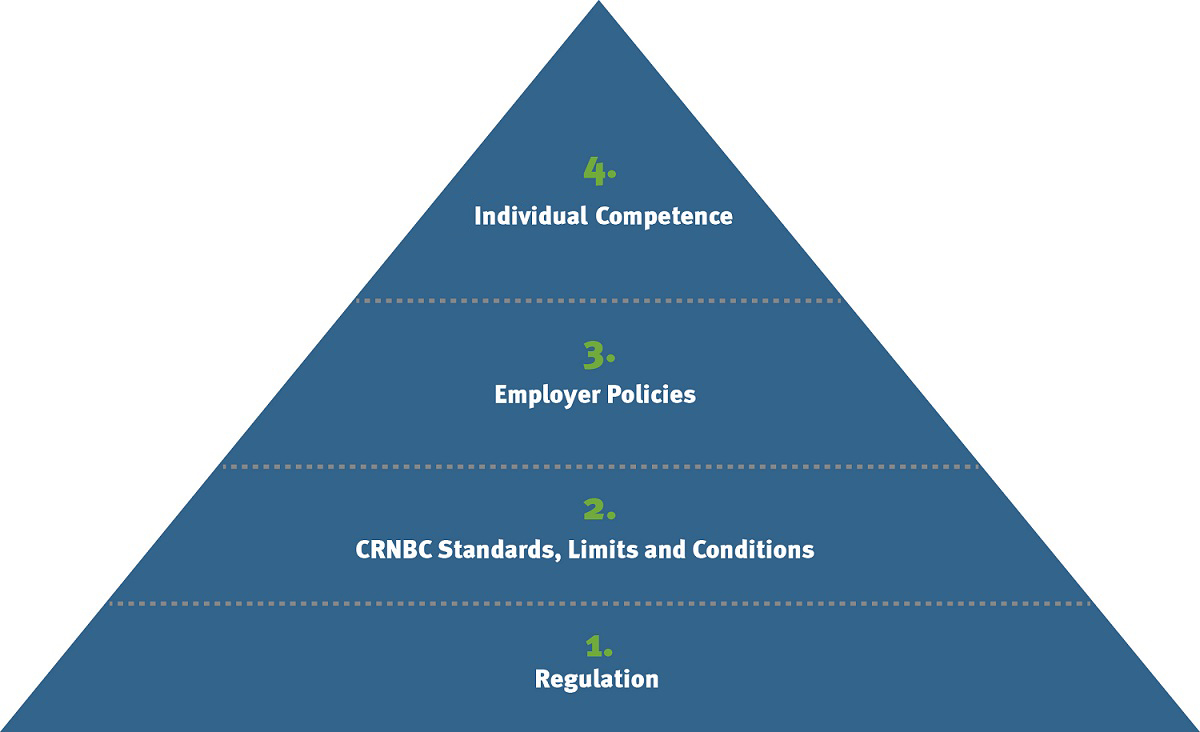
 What's My Role?
What's My Role?
Follow the best practice guidelines below when engaging directly with clients, conducting training with clients or patients, or distributing THN kits.
CLIENTS: Clients are those who are at risk of an opioid overdose or who have a friend or family member at risk of an overdose, and are seeking overdose prevention and Naloxone training, a THN kit or a THN refill.
- Learn and demonstrate knowledge of the six S.A.V.E. M.E. steps to respond to an opioid overdose
- When responding to a suspected overdose, always protect yourself by wearing gloves and using the face shield provided in the kit
- Watch for needles and other sharps on or around the scene
- Assist with helping the client access Opioid Agonist Therapy (OAT), shelters, and community harm-reduction services
TRAINERS: Trainers include those who do 1:1 client/patient training on overdose prevention and Naloxone administration, then distribute THN kits.
- Learn and demonstrate the six S.A.V.E. M.E. steps to respond to an opioid overdose, AND adhere to the additional “Quick and Dirty Tips for Trainers” found here
- Always wear personal protective equipment such as the face mask and gloves to protect you while administering Naloxone
- Watch for needles and other sharps, on or around the scene
- Special Considerations for those with CPR or First-Aid Training
- If the person or client you are training has CPR or first-aid training, they may have assessment and skills to intervene beyond the S.A.V.E. M.E. steps. In such cases, it is important to highlight that RESCUE BREATHS, rather than chest compressions should be used, to avoid putting the client at higher risk.
- If the overdose is unwitnessed, or if you are unsure if the client has a heartbeat, then chest compressions and breaths can be used, providing you have first aid training or are comfortable performing CPR.
 More Info
More Info
Opioid Overdose Information sheet (PDF)
Replacement Naloxone kits are available at community sites: towardtheheart.com or on the VCH website at vch.ca