Several factors can influence a drug overdose. The majority of fatal overdoses involve multiple substances – including alcohol and prescribed medications. Risks can be reduced by following some basic prevention and risk-reduction strategies.
 Three Key Things
Three Key Things
Multiple Substances
The majority of unintentional fatal overdoses involve combining multiple substances/alcohol/prescription drugs, which increase a person’s risk for having an overdose. For instance, mixing uppers and downers like benzodiazepines and alcohol, or cocaine and heroin compromises the body’s ability to maintain lifesaving functions.
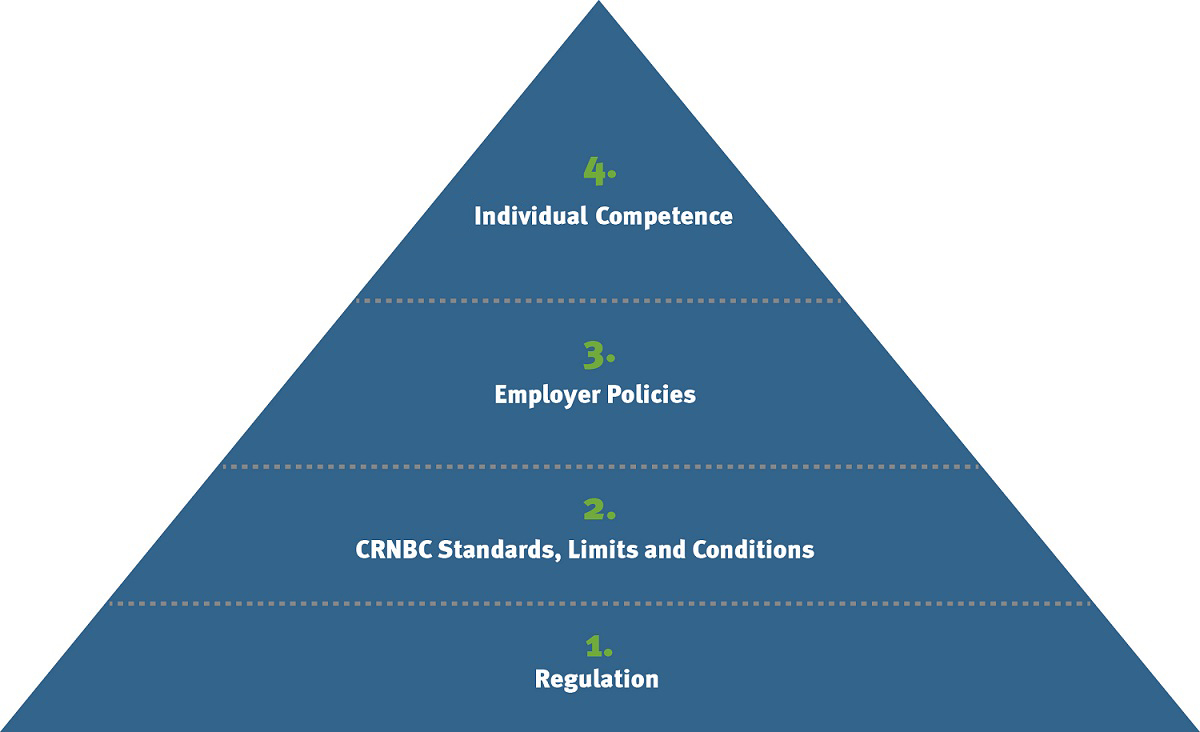
1 + 1 > 2
“Potentiation” is the term used to describe the unpredictable and increased risk when 2 or more substances are mixed, versus if one substance is taken on its own. We say that mixing two drugs is greater than the sum of its parts.
Risk of Using Alone
The highest percentage of deaths are occurring in people’s homes when they are using alone.
 Find Out More
Find Out More
Understand the risk factors that can lead to a drug overdose:
Quality, Cut or Toxicity (in an unregulated drug market, it is extremely difficult to know the amount of drug or contaminants in illicit substances.)
Illicit substances are not regulated in Canada, or in any other place in the world, so it’s impossible to know what contaminants/buffers have been cut into a drug. This poses a challenge for people who use drugs as there is no way to determine purity or dosage.
Tolerance
An individual’s tolerance to a drug decreases with a few days of non-use, or even of reduced amount per day. People who "relapse" after a period of not using drugs are at extremely high risk of fatal overdose.
Health Status
A person’s ability to eliminate substances from their system and, more importantly, their risk for having an overdose, is shaped by many health-related factors. People who are ill (e.g. from liver, lung or brain diseases) are at increased risk of a fatal overdose.
Genetic Factors
Every individual’s body breaks down drugs differently, depending on their unique genetic make-up. This means that one person may have a very different response to a drug than another person.
Route of Administration
The faster a drug hits the blood stream, the greater the risk of an overdose. Injecting drugs carries the highest risk of overdose. However, a person can still overdose, from smoking, inhaling/snorting, or swallowing a drug.
 In Practice
In Practice
John regularly injects street drugs such as crack cocaine, heroin and crystal meth, which can contain Fentanyl. Lately he has been forced to switch dealers. Fentanyl can be found in street drugs such as heroin, crack cocaine, and crystal meth. Switching dealers or finding a new drug supply has the potential of posing a high risk for overdose, due to the uncertainty of the strength of the new supply compared to the old supply.
Take a moment to consider what harm-reduction advice you might offer John.
You might ask John what he is doing to reduce his risk, advise him to start low and go slow, do a test dose or use less, and use at a supervised injection or overdose-prevention site.
Hmm... Actually, this is an example of when you might see an amount in your budget for Physician Compensation.
Donna has just arrived at your clinic. She tells you that she doesn’t think there’s any risk of overdosing if she uses opioids and stimulants together. People often think that mixing stimulants with a depressant will cancel out the risk of an overdose. However people who ‘speedball’ (mix) are at higher risk because the body has to process more drugs. Stimulants cause the body to use up more oxygen and depressants reduce the breathing rate.
What education points could you provide to Donna?
- Stimulants cause the body to use up more oxygen and depressants reduce the breathing rate. These drug mixes decrease your body’s ability to cope with an overdose
- Use Trauma Informed Practice (TIP) in your care
- Share information on not using alone, learning to recognize the signs of an overdose, learning to respond to an overdose, and the risk for other drugs to be contaminated with fentanyl
- Suggest or assist with improved care transitions by collaborating with other health care workers to provide the best client centred care
- Assist with access to Opioid replacement therapy, treatment, recovery and/or community harm-reduction services based on client directed needs such as (links to VCH resources to be added)
Hmm... Actually, this is an example of when you might see an amount in your budget for Physician Compensation.
 What's My Role?
What's My Role?
Work with clients to reduce overdose risk by:
- Using principles of trauma-informed practice to hold safe, respectful and non-stigmatizing conversations about drug use
- Discussing safer-use strategies such as: not using alone, using less, doing testers, and using alternate, safer routes of administration in order to decrease risk
- Assisting with accessing care and navigating healthcare systems
- Offering assistance to addiction services, Opioid Agonist Therapy (OAT), shelters, and community harm-reduction services